Engineers Develop New Portable Malaria Screening Instrument
According to the World Health Organization, over 216 million people were infected with malaria in 2016, and 445,000 individuals died from the disease. The key to solving this health crisis is early-stage diagnosis, when malaria therapeutics are most effective. A new prototype for a portable instrument capable of early-stage malaria detection has been developed by a team of researchers at the USC Viterbi School of Engineering.
There are two standard ways of diagnosing malaria—yet both have limitations. The first involves taking a blood sample and looking at it under a microscope to identify red blood cells that have been infected with the malaria parasite. This involves counting cells—which is manually intensive and dependent on the technician reading the blood smears. The second approach, known as the rapid diagnostic test (RDT), works in about 15 minutes. However, without refrigeration, RDTs can spoil like milk or eggs.
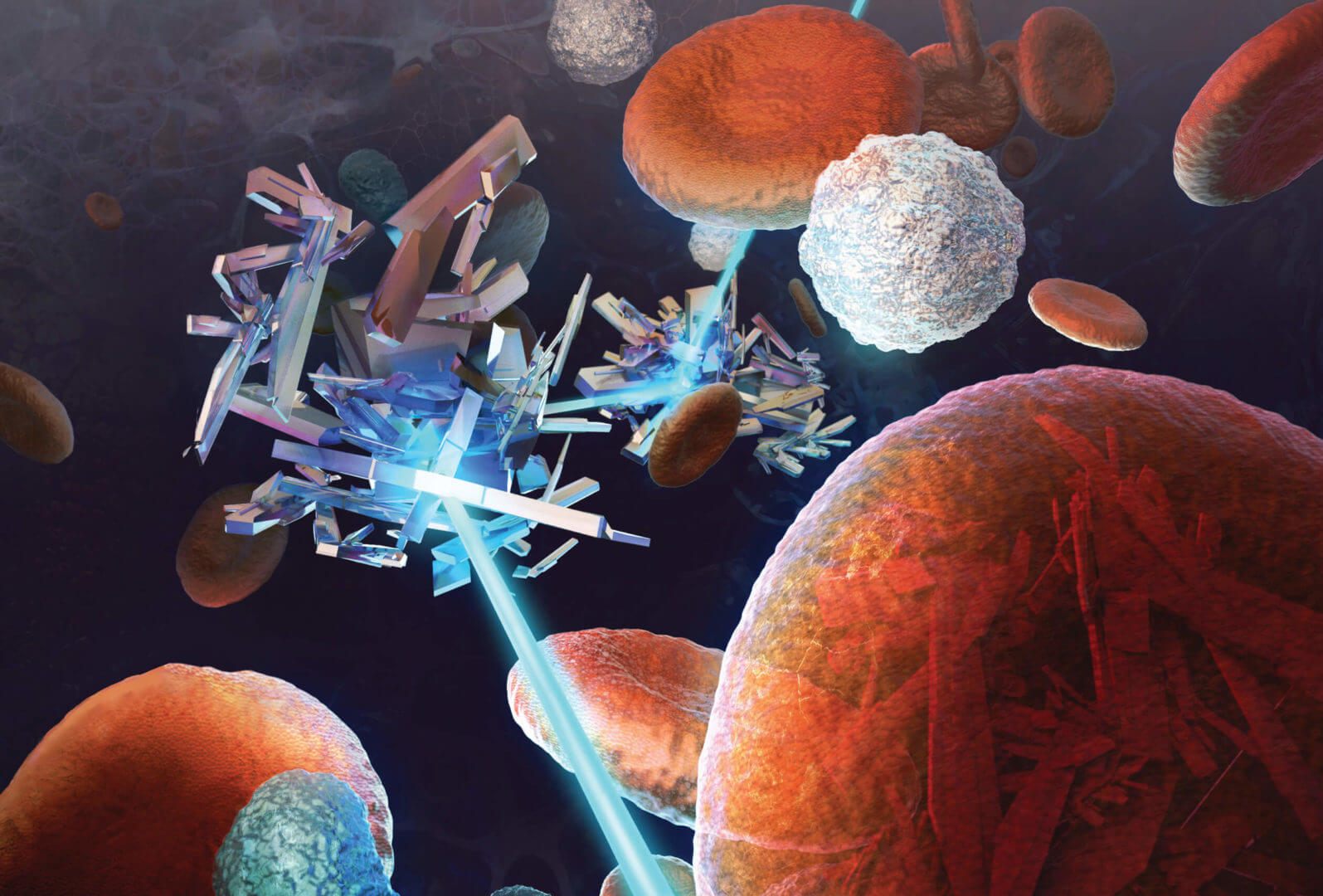
“Malaria primarily impacts low-resource environments where supply chain management is difficult and access to power can be unreliable. Therefore, an effective malaria diagnostic must be independent of these,” said corresponding author Andrea Armani, the Ray Irani Chair in Engineering and Materials Science, whose lab is located in the new USC Michelson Center for Convergent Bioscience.
Advantages of the PODS
The portable optical diagnostics system (PODS) prototype developed by USC Viterbi engineers Andrea Armani, Samantha McBirney, Dongyu Chen, and Alexis Scholtz, detects a by-product called hemozoin generated by all species of the malaria parasite. As such, it is a rapid screening for all malaria strains.
The PODS instrument was designed to solve the challenges limiting current systems. To minimize size, weight, and power requirements without sacrificing performance, every aspect was considered. The prototype weighs less than 10 pounds, is 12-by-10 inches (the size of a large shoebox) and can be powered by a battery for eight hours. In addition, PODS was designed to require minimal sample processing and handling, as well as to eliminate the need for secondary chemicals with strict storage requirements. This makes the device particularly suited to low-resource environments.
The current prototype can analyze an unprocessed, whole blood sample in 10 to 15 minutes. With only 500 µL of blood (five to seven drops), it can achieve sensitivity levels needed for an early-stage diagnosis.
“This could represent a tipping point in the global fight against malaria,” Armani said.
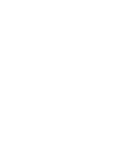
The laser beam passes through the blood sample and hits the detector on the other side. Two measurements are taken: one with the magnet next to the sample and one without the magnet. If there is any hemozoin in the blood, it will be pulled to the side of the sample holder by the magnet, changing the amount of light that can make it to the detector.
Malaria-infected mosquitoes infect human hosts with the parasite. Their primary nutrient source is hemoglobin, a component of red blood cells. As the parasite digests hemoglobin, it creates what is known as heme as a by-product.
PODS has three primary components: a laser, a detector (to detect light), and a magnet. When a sample of blood is placed between the laser and the detector, the amount of light that makes it to the detector decreases as the blood blocks it. If hemozoin is present, even less light shines through. At high concentrations even in blood, it is readily apparent if hemozoin is present because the nanocrystal is very good at blocking light. However, as the concentrations decrease to values indicative of early-stage malaria, it becomes harder to detect the presence of hemozoin. (Additionally, everyone’s blood absorbs light a little differently, further complicating the measurement.)
By applying a magnet, it is possible to manipulate and move the hemozoin particles within a test tube, or move them in and out of the laser beam. In this way, a single sample can be used to perform two measurements, and every diagnosis is personalized. If hemozoin is present, even in minute concentrations, the signals change. “PODS operates on a very simple design concept. If there is hemozoin, then there must be malaria,” Armani said.
Design Philosophy
The researchers intentionally designed the device to use inexpensive, off-the-shelf components and not require any reagents. If a component fails, the engineers wanted to ensure that it was not necessary to seek out a custom supplier or a single-source supplier.
“All the parts are readily accessible and easily replaced,” McBirney said.
The researchers are now working on the next generation of the device to improve its ruggedness and further reduce the sample volume to under 200 µL (one to two drops) of blood. They expect to eliminate the attached laptop so the device could operate for over 30 hours with an external battery pack or be hand-powered.
The article featuring this research, “Portable diagnostic for malaria detection
in low-resource settings,” is featured in ACS Sensors.