The Boy who Plays Baseball With Only Half a Brain
Rafael Hernandez shouldn’t be alive.
At four months old, he survived a horrific head-on collision with a semi. His father, Ralph Hernandez, a U.S. Marine, was killed on impact and ejected from the vehicle. When his mother, Mariza Hernandez, lifted Rafael out of the wreckage, his car seat split in half.
Rafael’s skull was extensively fractured. To save his life, doctors removed 46 percent of his brain, returning him to his mother in a vegetative state.
Secondary to his brain injury, Rafael developed dystonia — a neurological movement disorder that would further lock him inside his body, causing involuntary muscle spasms and painful, twisting movements.
“They told me he’ll never learn to sit or walk, feed himself or reach for objects,” Mariza Hernandez said. “He’d be legally blind and the grand mal seizures could eventually kill him.”
But Hernandez refused to believe the prognosis. She held on to hope for the next 23 years, through late-night ambulance rides, brain surgeries and violent seizures.
“He never gained more than 91 pounds,” she said. “For 21 years, not a pound over 91!”
Today, at 23 years old and 140 pounds, Rafael is full of life. He dances and sings and plays baseball. On August 5, his mother cheered him on as he pitched in the Little League World Series in front of ESPN cameras for the Azusa Challengers, a team made up of children and young adults with disabilities.
Rafael, whose name means “God healed,” did more than survive, thanks to his mother, who never gave up on him, and an emerging medical procedure called deep brain stimulation, or DBS. The procedure, which has been around for years, was re-designed and perfected by USC Viterbi professor Terence “Terry” Sanger and other researchers willing to cross paths and disciplines at USC Viterbi, Children’s Hospital Los Angeles and the Keck School of Medicine of USC. That group included electrical, mechanical and biomedical engineers; data scientists; nurse practitioners; physical therapists and some prominent names in neurosurgery, including Mark Liker, Aaron Robison and Mark Krieger.
This is their story. And the story of patients like Rafael whose lives were transformed by DBS. The story of what happens when medicine and engineering converge upon the human brain. A story a decade in the making to bring healing to children and adults imprisoned by their own bodies.
The Good Doctor And His Mortal Enemy
Doctors who specialize in children’s movement disorders are rare. Of these, according to neurosurgeon Liker, Sanger is one of the top three.
Sanger, a provost associate professor of biomedical engineering, neurology and biokinesiology at USC Viterbi and the Keck School of Medicine, has treated hundreds of children suffering from the worst neurological disorders, mostly at CHLA.
“What makes Dr. Sanger unique in the medical world is that in addition to being a child neurologist, he’s also an electrical engineer and computational neuroscientist,” said Liker, a clinical assistant professor of neurosurgery at the Keck School.
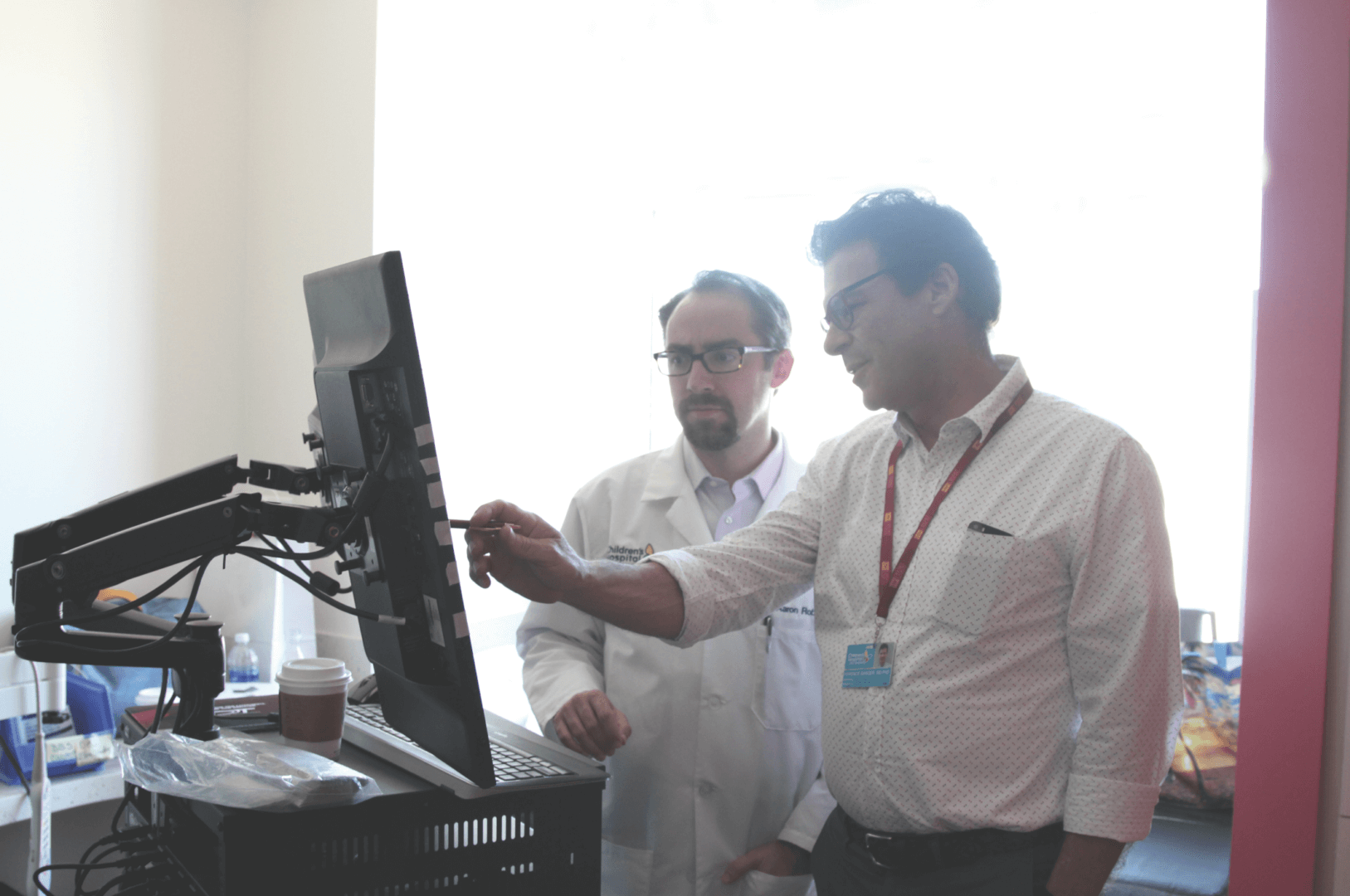
“His background allows him to look at a long-standing puzzle in the human brain,” said Robison, a neurosurgeon at CHLA and assistant professor of clinical neurological surgery at the Keck School. “How do you take individual neurons firing inside their networks — from the cortex to the basal ganglia to the spinal cord — and try to figure out how the brain encodes this information? It’s a coding puzzle that no one has solved.”
Sanger founded the USC Health, Technology and Engineering Program (HTE@USC) and the Sanger Lab, where he uses engineering to understand childhood movement, discover treatments and enable novel devices like exoskeletons and artificial spinal cords. Indeed, the Iron Man analogy isn’t too farfetched if you’re a child sitting in Sanger’s lab watching him remotely control a robotic arm using only his forearm muscles.
His mortal enemy? Dystonia.
“I see a lot of kids with lots of different movement disorders, but dystonia is probably the most common, and one of the most frustrating because the children are very locked in,” Sanger said.
Some of the children in Sanger’s care have their arms tied down to their wheelchairs so they don’t hurt themselves involuntarily. Others crawl crablike on the floor.
“It’s not just that they can’t move or can’t get what they want,” Sanger said. “In many cases their cognitive functions are perfectly normal. They know what’s going on — they want to communicate, they want to move, but their bodies won’t let them.”
Since officially starting the DBS program at CHLA seven years ago, Sanger has seen children stand up out of their wheelchairs and walk again. Children whose arms flailed so uncontrollably that they routinely dislocated their shoulders are now able to ride a bicycle. Children whose torsos were painfully bent at a 90-degree angle to their hips can now sit up straight.
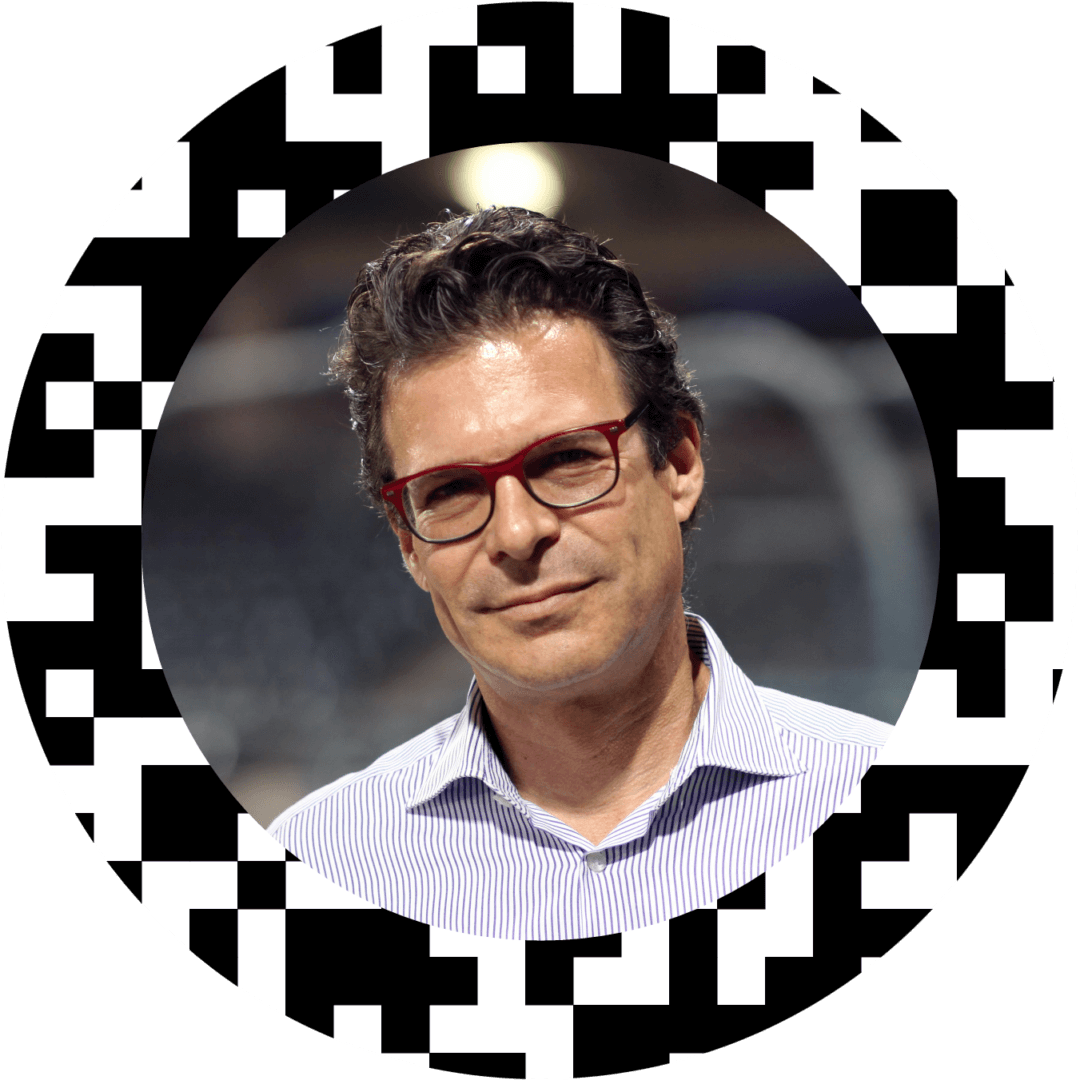
DBS — literally drilling into patients’ skulls and zapping the deepest structures of their brains with electricity — has been around for a while. In fact, electrical stimulation of the brain was first applied in a human by Roberts Bartholow in 1874. The modern era of DBS began in 1987 when Alim Benabid published a landmark paper reporting on the use of ventral intermediate nucleus (VIM) stimulation to treat tremor. It has since been used to treat more than 40,000 people with Parkinson’s and essential tremor worldwide, and is currently undergoing clinical trials as a treatment for depression and obsessive-compulsive disorder.
In the summer of 2016, Sanger’s team discovered a much more targeted way of treating children and adults with dystonia. Robison had developed a surgical technique for inserting temporary electrodes to stimulate the deep structures of the brain, based on his prior experience with epilepsy surgery — all while simultaneously recording brain activity from micro electrodes, microscopic wires capable of detecting the activity of individual neurons. Sanger created a whole new testing regime with new data analysis techniques, and since then, they’ve amassed the largest data set of the diseased brain ever assembled. Not only is it improving the lives of kids, it’s opening up a new frontier of research for doctors and clinicians all over the world.
Unlocking Bodies Trapped by the Brain
What allows Rafael Hernandez to pitch a baseball and control his body despite missing nearly half of his brain are two thin wires with four electrical contacts at their tips, sending a finely tuned electrical pulse into a very specific and carefully selected region of his brain. Neurosurgeons Liker and Krieger performed the surgery while Sanger guided them to the exact targets.

This wire, called the DBS lead, reaches the deepest recesses of Rafael’s brain — the globus pallidus and the thalamus. The wire is connected to a pacemaker-like device implanted in Rafael’s chest below his collarbone. This device, called the neurostimulator or implantable pulse generator (IPG), contains the battery and computer source that generates the electrical pulses delivered via the lead to the brain.
No one knows exactly how DBS works, although Sanger is trying to find out. He believes that the electrical impulses from the battery cause nerve cells to fire in a group, and this effectively overrides the abnormal signal patterns coming through those nerve cells. In effect, DBS substitutes a benign and somewhat boring pattern of neural firing for the disabling pattern that creates dystonia. Over time, the brain adapts to the artificial DBS stimulation by turning down the volume on the boring pattern of activity, which further blocks the dystonic signals from getting through.
How DBS Works
Sanger stresses that dystonia is a symptom, not a disease. Something else is going on deep in the brain that is the underlying cause.
“Dystonia co-opts the normal control mechanisms of the brain,” Sanger explained. “The reason this is important to know is because you’re trying to say where does this come from. It’s not coming from the low levels of the motor system, the things that cause, say, muscle twitches. It’s coming from the things that control posture and movement.”
What Sanger and others do know is that faulty signals from the brain cause muscles to spasm and pull the body into twisting, repetitive movements or abnormal postures. It can be caused by an inherited gene, damage to the central nervous system or birth trauma. But in many cases dystonia appears seemingly out of nowhere. It can affect a single muscle, a muscle group, or extend to the entire body. Some early symptoms can include a “dragging leg,” cramping feet, involuntary pulling of the neck, uncontrollable blinking and speech difficulties. As many as 250,000 people in the United States have dystonia, according to the American Association of Neurological Surgeons, making it the third-most common movement disorder behind Parkinson’s.
Neurologists typically split dystonia into two categories: primary or genetic dystonia, and secondary or acquired dystonia — like Rafael’s — caused by trauma to the brain or another condition such as cerebral palsy and certain kinds of poisoning and biochemical diseases. Inherited dystonias are rare compared to acquired dystonias.
Rafael’s recovery is even more miraculous considering DBS has only recently been used to treat people with acquired dystonia. DBS has been approved by the Food and Drug Administration to treat Parkinson’s since 1997, and it has a humanitarian device exemption to treat inherited dystonia. But patients seeking DBS for acquired dystonia do so off label.
Studies suggest that only about 50 percent of children with acquired dystonia see a significant benefit from DBS. But Sanger and his team have recognized a significant benefit in over 70 percent of these children.
“For my son, it’s been 110 percent improvement,” Mariza Hernandez said. “Since DBS, Rafael has also been seizure free.”
For children suffering from inherited dystonia, the frightening symptoms hit at a crucial time in their development.
The Girl Whose Hand Forgot What It’s Supposed To Do
Jordon Bautista’s dystonia appeared when she was a first-grader in Whittier, California. But it took six years for a correct diagnosis.
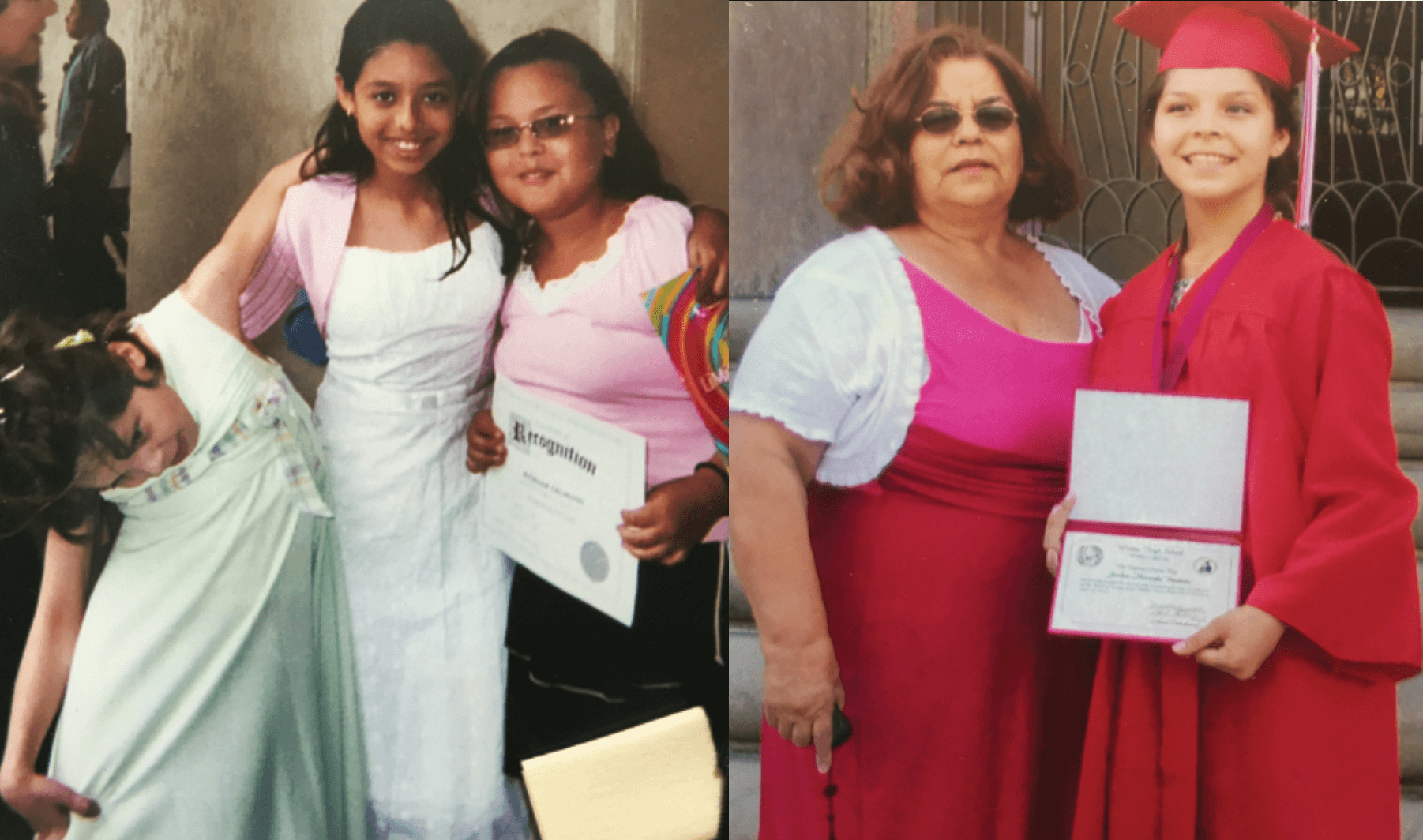
“I would write and then all of a sudden my hand would jerk out,” said Bautista, now 22. “I would disassociate my body parts. I’d say, ‘It doesn’t want to,’ because it had a mind of its own. I would literally look at my hand and be like, write. And I couldn’t.”
At first, her parents and teachers thought she was faking it. “‘Here goes Madam President again,” they said. “Always in need of attention.”
Confused and in pain, she taught herself to write left-handed. Then the dystonia moved to her shoulder. Her neck muscles started to twitch and pull her head to the side.
“I had to prop my head up with my knee so I could do my homework,” Bautista said. “I was putting so much pressure on my temple that it left an indentation in my skull.” Early doctor visits showed nothing abnormal in Bautista’s brain. Some in her family began to think her condition was all in her head.
As the months became years and her condition worsened, she played down the problem until gradually her upper body froze sideways at a rigid 90-degree curvature, and she had to be strapped to a wheelchair. “My head was literally where my knees were,” Bautista said.
For Bautista, living with dystonia meant learning to live in a new body. It also meant learning to manage a great deal of pain.
“When kids at school would stare at me, I’d make a weird face at them and say, ‘I’m a pirate! Argh!’” Living with dystonia also gave her an endless supply of shrewd quips.
Doctors usually treat dystonia with a three-tiered approach: botulinum toxin (Botox) injections, several types of medication and surgery, alone or in combination. Medications and Botox helped block the communication between the nerves and muscles to reduce Bautista’s abnormal movements and postures. But drugs also affected her at school.
“Compared to medicine, which bathes the entire brain in a chemical, DBS is much more precise,” Sanger said. “With a tip of an electrode we’re stimulating millions of cells.”
Six years after her symptoms appeared, Bautista was cleared for DBS in 2008 by Jennifer S. Hui, director of the DBS program at Keck Hospital. Bautista has a vivid memory of the surgery and the “army of white lab coats” congregating to get a good look at her. They’d never seen a case quite like hers. In fact, Bautista’s was the first DBS procedure done at CHLA, with Mark Liker operating.
“I’ll never forget her,” Liker said. “Here was this funny, bright, 12-year-old girl bent at a 90-degree angle to her hips with severe scoliosis. She was in a lot of pain.”
Bautista underwent the standard procedure at the time usually done on Parkinson’s patients, in which two permanent wires are placed into the brain in a single surgery. Liker, who has performed hundreds of DBS procedures in Parkinson’s patients since 2002, and in children with inherited as well as acquired dystonia since 2006, was tasked with planning a trajectory around blood vessels and critical structures in Bautista’s brain before inserting the permanent leads.
“Unlike most open brain surgeries, where everything you’re doing is right there in front of you and you can see it, we’re operating on the unseen brain, because we don’t see the brain at any point during the procedure,” explained Robison, who now performs these surgeries alongside Liker at CHLA. “In many ways, it’s an invisible surgery.”
But with Sanger’s arrival, these risks are mitigated with a lot of data. With his procedure, after a child goes under anesthesia, neurosurgeons insert up to 10 temporary leads in five different areas of the brain. Then they wake up the patient. The child stays in the hospital for the next seven days while the temporary leads implanted in their brain record neural activity. They can sit up sit up, play cards, draw, even drive their electric wheelchairs around their hospital bed. Each wire in the child’s brain can have up to 16 little contacts on it, recording the brain on 160 channels.
“We’re listening to the cells,” Sanger said. “And we see particular brain areas fire like crazy every time the child has spasms. So that’s telling us, OK, now we need to figure it out where these are coming from so we can stimulate those areas and turn off the dystonia.”
The broken brain is giving Sanger a snapshot, little clues of information he can piece together, correlated against the muscle activity and what the child is doing. Sanger is not trying to cure a disorder that occurs while the child is lying flat on her back in the operating room. He gets to see what these children want to do, the problem they’re having performing that function, and what their brains are doing at the exact moment they’re having this problem, and he uncovers the pattern.
For Bautista, the results were astounding.
“She’s beautiful. She has a boyfriend. She’s living a full life. If you see her walk into a room today you wouldn’t recognize her,” Liker said.
She is now a teacher’s assistant for children with disabilities at the same elementary school she attended.
“The teachers can’t believe it’s me,” she said.
She’s also thinking about marriage, about a career as a special needs teacher and about becoming a spokesperson for young people with dystonia.
When you ask Bautista what she appreciates most of all from her life now, she said, ‘Walking! Walking straight. Walking right. Walking upwards instead of sideways. Freedom. You know … I was trapped in a body that I didn’t belong in.”
The Final Frontier
The research continues deep in the Sanger Lab, where USC Viterbi Ph.D. candidate Enrique Argüelles and postdoctoral research associate Arash Maskooki listen to scratchy white noise coming in and out in bursts. It sounds like a distant satellite sending some extraterrestrial transmission.
What they’re listening to is a real-time soundtrack of a living human brain, up to 250 different neurons in the deepest areas in the dystonic brain of one of Sanger’s upcoming surgery patients. The activity is projected on a screen, giving them a colorful visual of the patterns the brain uses to select and control movement.
Like a child trying to get attention, the symptom gets louder and louder, the signal coming across with ever increasing voltage and violence. Treating the brain, it seems, is largely the art of listening.
“This is how we figure out where to implant the DBS wires into the brain,” Maskooki explained. “It tells us what patterns we need to block or change in order to improve movement.”
Like an electronic device, information in our brain is encoded, processed and transmitted electronically. The neurotransmitters, which are the basis for most pharmacology, are just the messengers between the neurons — they are not the message. The message, or code for how the brain commands specific types of movements and postures, remains a puzzle.
A child’s brain generates about 4 to 5 terabytes of data during the weeklong recording that happens prior to inserting the permanent DBS leads — the equivalent of 1,250 feature-length movies — everything from movement to what happens in the brain during sleep or while drawing. Sanger’s team has the capacity to do 10 DBS cases a year — and at 5 terabytes per case, that’s 50 terabytes.
He is eager to open up this data trove to other scientists. But over a high-speed American internet connection, a year’s worth of DBS data can take up to two months to download. The only way around it is to do some fancy storage and compression and distribute data to scientists only when they need it for their particular research.
“It’s essentially an unsolved computer science problem,” Sanger said. “There has never been a data set like this of the human brain.”
His team is now devising a better way to perform the procedure both in terms of safety and flexibility. Eventually, once they have a proven concept, the procedure can easily be ported to other centers.
“This is much better than what we had before,” Sanger said. “It’s huge amounts of data, but it’s nowhere near the brain itself. I may have 160 wires in the brain. The brain has 85 to 100 billion neurons. I’m off by a little bit.”
Still, it doesn’t stop Sanger from pursuing the broken brain’s secrets. And the more broken a brain is, that’s where you’ll find him, seeing opportunities where others see only confusion.
“For me,” Sanger said, “if you’re going to spend your life investigating a disease, you should investigate something that’s not yet treatable but for which there exists a potential for significant benefit.”
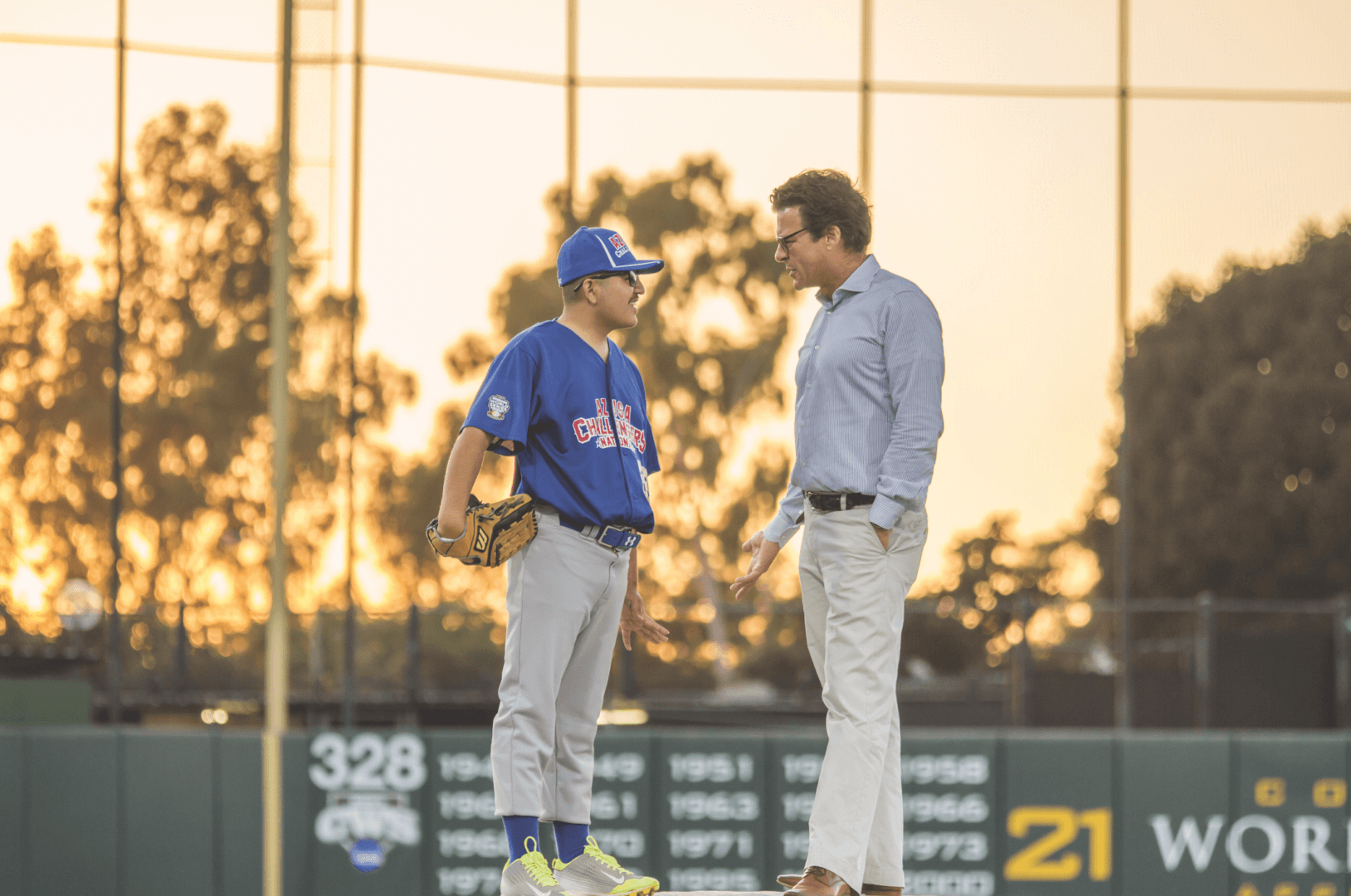
On August 21, Sanger and Rafael Hernandez had a reunion on USC’s Dedeaux Field. Four years had gone by since Rafael’s procedure, and Sanger, who hadn’t seen Rafael since, came out to watch him pitch. They even played catch together.
For Sanger, it was a rare occasion to witness the long-term effects of DBS.
“Did I surprise you?” Rafael asked him after inquiring about how Sanger’s family was doing.
“Yes, you’ve changed so much. You’re all grown up now,” Sanger answered.
“I want you to always remember me right here,” Rafael said, pointing to Sanger’s heart. “Right here! And whatever happens, I always got your back, Dr. Sanger. You’re my homeboy!”
The moment was not lost on Sanger, who turned to a teary-eyed Mariza Hernandez and said, almost to himself, “This is why I do this.”
The Patients
Kylee Jane Young
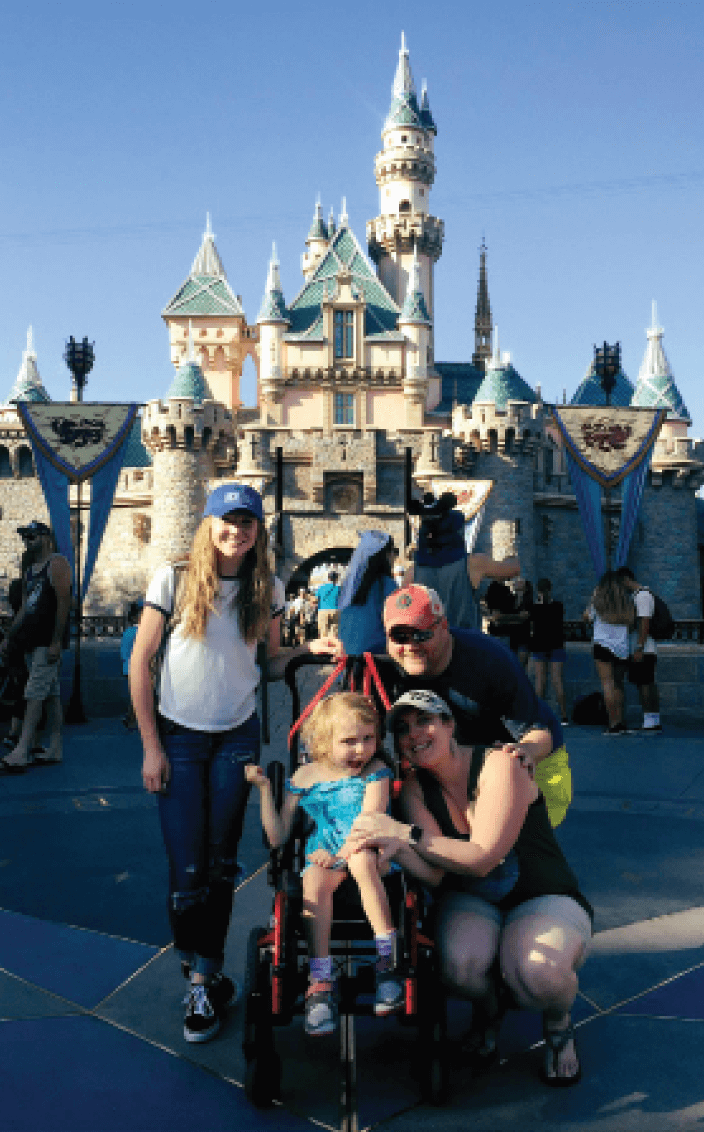
Hometown: Ridgefield, Washington
Age: 7
When Kylee was 2, she contracted a bacterial infection that threw her body into septic shock and caused a major stroke. Her mother, Jill Brown, donated her own kidney to save Kylee’s life. But the stroke severely impaired Kylee’s motor functions, and over time she developed severe dystonia. Since she underwent the DBS procedure, she is able to attend second grade
in a typical class, go to Girl Scout camp, and loves to go swimming.
“I can see her growing up so much straighter and stronger than before,” said Jill Brown. “Right now, she’s just being a kid, having fun and making friends. I’m so proud of her!”
Samantha “Sam” Durham
Hometown: Arroyo Grande, California
Age: 18
Sam’s parents couldn’t figure out what was wrong with their 18-month-old daughter. She wasn’t gaining any weight, so they took her to the hospital, where a CT scan revealed a brain stem tumor the size of her fist. Doctors removed the tumor but damaged Sam’s brain stem in the process. Following several unsuccessful surgeries and a stroke, Sam lost all movement on her left side. She was confined to an electric chair in a posture that was becoming more and more twisted as she grew older. Now with DBS, Sam looks forward to enrolling in college. She loves to write poetry and draw. Here’s an excerpt from short poem she wrote while undergoing DBS surgery at CHLA:
“I think about rainbows and trees
And clouds in the sky
And I say it’s a beautiful thing.”
David Dewsnap
Hometown: Woodland Hills, California
Age: 54
Just being able to walk and interact with people is a great gift for David Dewsnap, Ph.D., whose career as a university professor of mathematics at Southeastern Oklahoma State University was interrupted by Parkinson’s disease. Holding a cup of coffee became a near impossible task. In a short time, Dewsnap lost his ability to speak, then his ability to walk. His symptoms were so powerful that they were resistant to standard treatments, so DBS became the only option. He now works as an actuary for AIG and is often invited on radio programs to talk about his DBS experience.
“It has given me my life back,” he said. “This procedure has been just amazing for me. Without seeing me before, you don’t really understand what it was like. I really couldn’t use the left side of my body.”