Somewhere Over the Rainbow: A Cancer Detection Powerhouse
Cristina Zavaleta was sitting in an animation class with artists from Pixar’s studio in Emeryville, California, looking at the candy-colored paints and inks they were using, when inspiration struck.
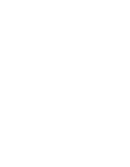
Zavaleta, the WiSE Gabilan assistant professor in USC Viterbi’s Department of Biomedical Engineering, works on imaging methods for cancer using nanoparticles that target tumors. With interests in art and animation as well, she was on the lookout for brightly colored imaging contrast agents that could be used to better illuminate and detect cancer cells.
“I was thinking about how these really high-pigment paints, like gouache watercolors, were bright in a way I hadn’t seen before, and I was wondering if they had interesting optical properties,” Zavaleta said.
The bright idea led her to Adam Sky, a tattoo artist in San Francisco, who also works with color-rich dyes.
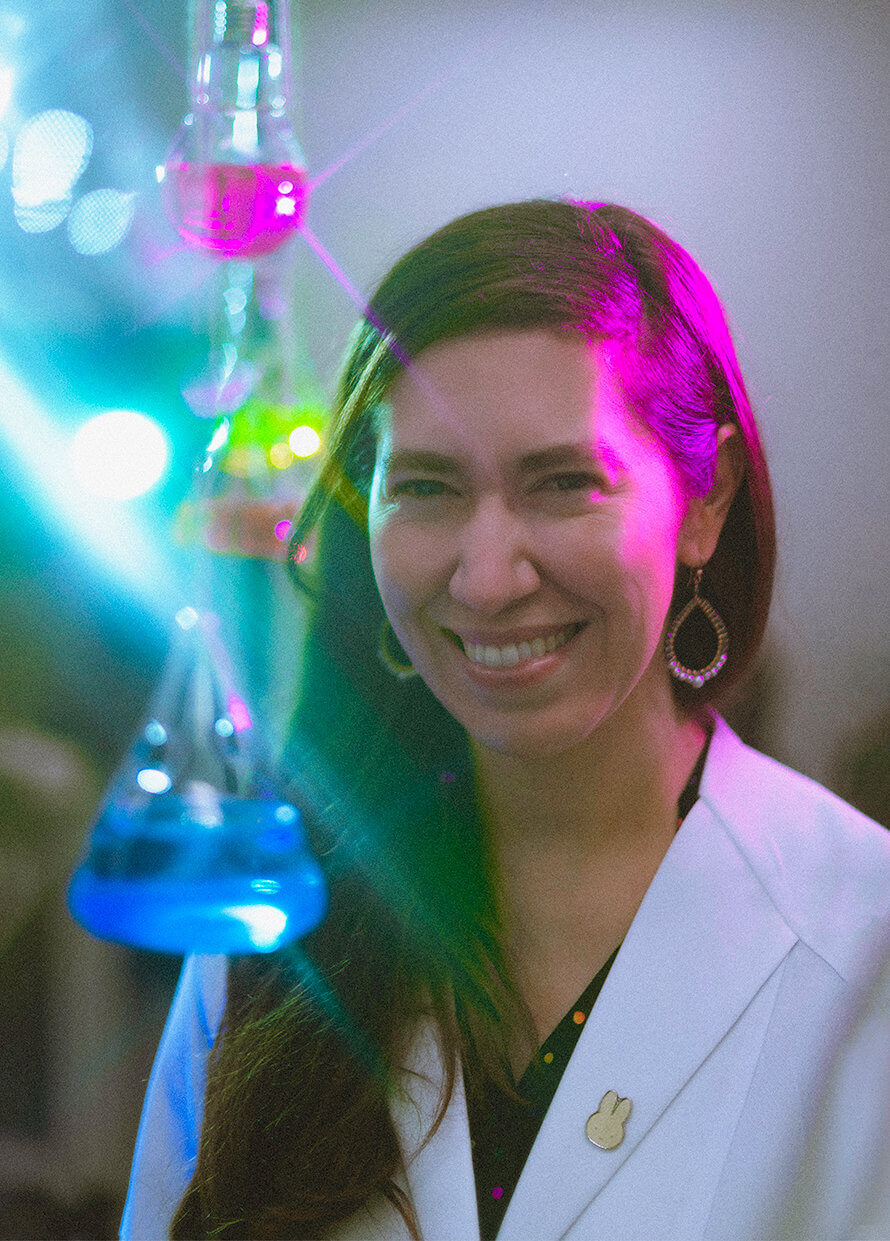
“I remember I brought a 96-well plate and he squirted tattoo ink into each of the wells,” Zavaleta said. “Then I took the colorful inks to our Raman scanner, which is used to sensitively detect our tumor-targeting nanoparticles, and discovered these really amazing spectral fingerprints that we could use to barcode our nanoparticles. It was super cool.”
Zavaleta and her team took this inspiration and developed new imaging contrast agents using common dyes such as tattoo ink and food dyes. When these are attached to nanoparticles, they can illuminate some cancers, allowing medical professionals to better differentiate between cancer cells and normal adjacent cells. Their work has been published in Biomaterials Science.
Early detection is crucial for patients to have the best possible outcomes from cancer, a disease that will affect over 38% of Americans at some point in their lifetime. Although there are several commonly used cancer imaging tools, such as MRI and CT scans, it is still difficult to detect cancer accurately and with precision. Imaging agents can improve the detection of cancer — these small-molecule materials, when injected into the body, can provide enhanced imaging contrast to help medical professionals identify and isolate tumors.
“For instance, if the problem is colon cancer, this is currently detected via endoscopy,” Zavaleta explained. “But an endoscope is literally just a flashlight on the end of a stick, so it will only give information about the structure of the colon — you can see a polyp and know you need to take a biopsy. But if we could provide new imaging agents to help doctors see whether that particular polyp is cancerous or just benign, they could avoid taking the biopsy altogether.”
To achieve this, the team has identified a unique source of optical contrasting agents from household coloring dyes and pigments already approved by the U.S. Food and Drug Administration — such as the dyes found in candies like Skittles and M&Ms — which the team hopes may allow them to be more easily and safely implemented in imaging practice.
These “optical inks” can be attached to cancer-targeting nanoparticles to improve tumor detection and localization. However, one of the challenges of imaging using nanoparticles is that they can have prolonged retention in organs like the liver and the spleen, which are responsible for trying to break them down. As a result, it’s crucial to consider biodegradable nanomaterials. Currently, there are a limited number of optical contrast agents approved for clinical use.
“We thought, let’s look at some of the FDA-approved drug, cosmetic and food dyes that exist and see what optical properties are exhibited among those dyes,” Zavaleta said. “And so that’s where we ended up finding that many of these FDA-approved dyes have interesting optical properties that we could exploit for imaging.”
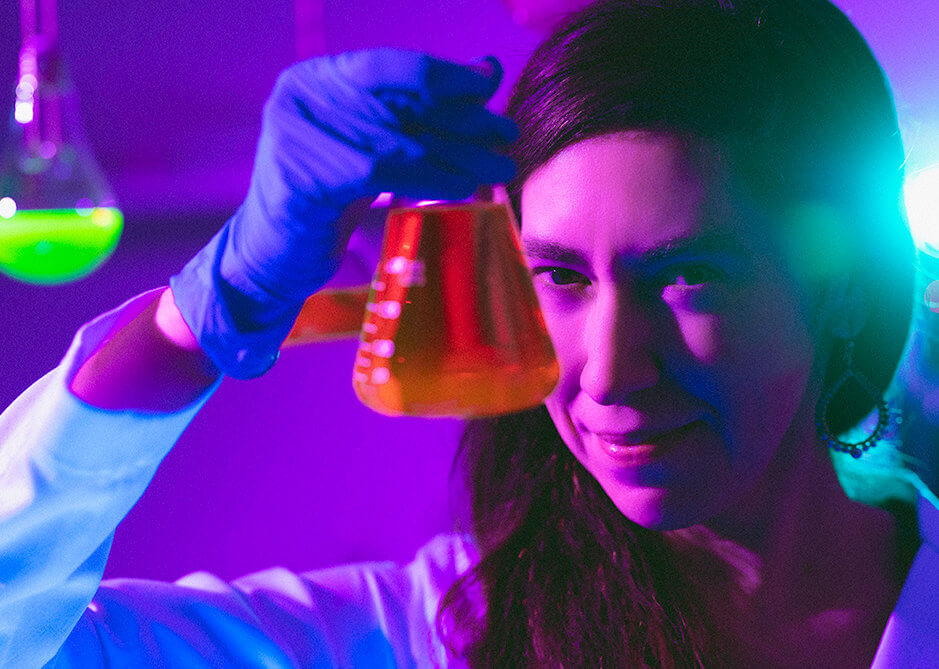
The team has developed a nanoparticle that will carry these highly pigmented imaging agents as a “payload,” ¬that is, an attachment to the particles. Zavaleta noted that the particles are of a specific size that enables them to passively penetrate tumor areas but can also be retained.
Most of the imaging contrast agents used today are so-called small-molecule dyes. “With small molecules, you may be able to see them accumulate in tumor areas initially, but you’d have to be quick before they end up leaving the tumor area to be excreted,” Zavaleta said. “Our nanoparticles happen to be small enough to seep through, but at the same time big enough to be retained in the tumor, and that’s what we call the enhanced permeability and retention effect.”
The nanoparticle can also be “decorated” with a larger payload of the dye than previous small-molecule imaging agents, which the team has shown under fluorescence imaging leads to brighter signal and significant localization of the nanoparticles in tumors.
“If you encapsulate a bunch of dyes in a nanoparticle, you’re going to be able to see it better because it is going to be brighter,” Zavaleta said. “It’s like using a packet of dyes rather than just one single dye.”
The research was co-authored by Helen Salinas, Dominie Miyasato, Olga Eremina, Rodolfo Perez, Karen Gonzalez, Alexander Czaja, Sean Burkitt, Arjun Aron, Augusta Fernando, Lauro Ojeda, Kimberly Larson, Ahmed Mohamed and Jos Campbell from USC Viterbi Department of Biomedical Engineering, and Beth A. Goins from University of Texas Health Science Center.