Army of Me
In 2018, new mom Julie Clauer was worried she wouldn’t live to see her 7-month-old daughter Liana’s first birthday.
Clauer had symptoms that at first felt like postpartum exhaustion. But when the fatigue and gastrointestinal issues worsened, she went to the ER. The true diagnosis spun Clauer into a new nightmare: She had stage 4 colon cancer that had metastasized and spread to her liver. It would later move to other areas, including her lungs and bones.
During those dark days, she could hardly have imagined herself hiking on vacation in 2023, with little evidence of illness, feeling better than she had in five years.
Since 2020, Clauer has participated in patient trials at USC Norris Comprehensive Cancer Center, combining immunotherapy with chemotherapy. Immunotherapy taps into the extraordinary power of the patient’s own body, activating the immune system to destroy cancer cells. Over time, the treatments have been effective in keeping Clauer’s disease progression at bay, shrinking her tumors and allowing for surgical options to excise the cancerous tissue — surgery that would otherwise not have been possible.
“I was shocked at the diagnosis. The prognosis wasn’t good. If I’d have looked it up, I probably would have been even more scared,” Clauer said.
Clauer was facing microsatellite stable, or MSS, colon cancer. MSS presents challenges because its tumors are considered “cold” — surrounded by a micro-environment of cells that suppress the body’s immune responses, often rendering immunotherapy ineffective. Stage 4 MSS patients often have few treatment paths beyond palliative care.
She began a whirlwind tour of oncologists to find someone willing to hit the front lines with her against this disease. She found exactly that in Heinz-Josef Lenz, the deputy director for research programs at USC Norris. Lenz leads numerous clinical trials investigating the new frontier of cancer immunotherapy.
Clauer moved her family from Chicago to Los Angeles, where she had grown up, and began treatment. But after two years of chemotherapy, surgeries and radiation, Clauer’s progress stalled, amid punishing side effects. Lenz encouraged her to participate in the combination chemotherapy/immunotherapy trial involving immune checkpoint inhibitors. This therapy targets the immune checkpoints that stop a patient’s body from recognizing cancer cells as foreign, triggering the T-cells to fight back.
It was a bold plan. Currently, immunotherapy is dependent on the patient’s immune response, and doesn’t work for every cancer. Only around 30% of patients were seeing disease control and stability on the trial in which Clauer enrolled.
“Immunotherapy has a less toxic profile, and we went into that trial with the goal of giving my body a break,” Clauer said. “Dr. Lenz has a very optimistic attitude. So even though he was not sugar-coating, his belief is that anybody can be an outlier. Anybody could be the one that has success.”
Clauer soon discovered she was an outlier.
“At the moment, she has basically no evidence of disease based on our immunotherapy. And she was not in our immune-responsive subgroup,” Lenz said.
After some initial side effects, Clauer’s scans showed significant shrinkage of her cancer. She went from having 11 lung tumors to four, which could be surgically removed.
“But then, when she eventually had tumor growth again, we changed our immunotherapy, based on our own understanding, to a novel combination, and she responded again,” Lenz said. “So, she’s in a very lucky situation. She is more than five years out from her metastatic disease, with no evidence of disease.”
Future scans will detect any tumor recurrences, but for now things are great. Clauer’s bloodwork is good. She enjoyed an active vacation with her family in Arizona where she saw the Grand Canyon for the first time. She is about to celebrate her daughter’s sixth birthday. Clauer’s progress meant she could pause the chemotherapy component of the treatment. She has been on immunotherapy alone since March.
“I have had no new side effects since then. My tumor is gone. It’s kind of remarkable,” Clauer said.
Immuno-engineering: A Powerful New Weapon
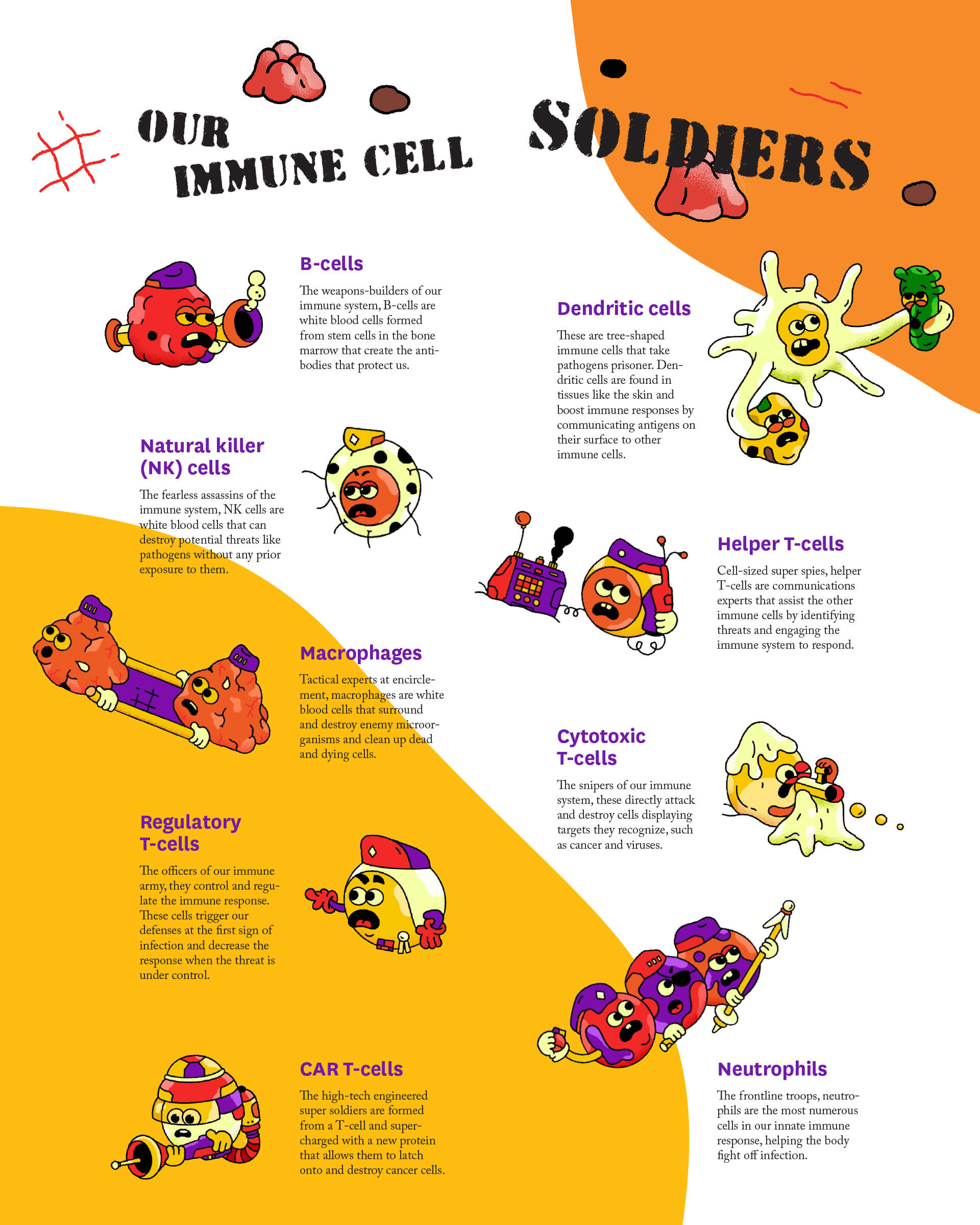
It may sound like something from the pages of science fiction: extracting immune cells directly from a patient, genetically engineering them to improve their performance, and putting those supercharged cells back into the patient. The result is a highly personalized treatment designed to detect and destroy cancer cells and other invaders with fewer side effects.
Immuno-engineering is the new super weapon in the fight against the world’s most urgent medical challenges, from cancer to viral disease and autoimmune conditions, even aging. These future therapies will build an exciting new arsenal for cancer patients.
Peter Yingxiao Wang is an expert in these cutting-edge cell-based cancer therapies. In 2023, he became the new chair of the Alfred E. Mann Department of Biomedical Engineering at USC, with a singular vision to expand the department’s significant strength in immuno-engineering.
Wang’s work lives in the exciting realm of chimeric antigen receptor (CAR) T-cell therapy, a revolutionary cancer treatment in which T-cells — a type of white blood cell — are given a unique protein receptor (CAR) that binds to cancer cells and allows the T-cells to destroy them.
Wang and his collaborators developed a breakthrough therapy that turns these CAR T-cells into remote-controlled attack drones. Wang’s team uses focused ultrasound to control the cells, known as FUS-CAR T-cells, to target and destroy solid tumors with greater precision, in a way that won’t impact healthy tissue.
“With chemotherapy and radiotherapy, often when they do work, they aren’t a complete remedy,” Wang explained. “Essentially the patient will survive somewhat longer, but eventually they will have a relapse. With immune therapies, particularly a CAR T approach, these T-cells can last for years. They can also suppress the tumor to stop a relapse. They allow the patient to live free of cancer.”
While CAR T-cell therapies are already changing the game in “liquid” cancers, such as leukemia, the challenge is making them work for solid cancers, where the CAR T-cell often has trouble penetrating the tumor’s suppressive microenvironment. You can adjust the expression of the CAR to make it stronger but run the risk of the cells attacking healthy tissue. Alternatively, releasing weaker CAR T-cells risks them being less efficient in killing tumors.
Wang’s team’s focused ultrasound CAR T-cells aim to address this challenge by only activating where the ultrasound directs them.
“You can isolate this tumor region to control it so that the CAR T will only be activated around the tumor. When the cells leave the activation zone, they lose function,” Wang said. “You isolate the problem, and you can use the strongest CAR without worrying that they may cause toxicity in other parts of the body.”
Wang and his team are now working with clinicians in the Catherine and Joseph Aresty Department of Urology of the Keck School of Medicine of USC with the aim of securing approval for clinical trials of the technology for prostate cancer.
In addition to Wang’s latest work, USC Viterbi has a solid track record in cell-based engineering technology:
- The Center for ImmunoEngineering, led by Pin Wang, Zohrab A. Kaprielian Fellow in Engineering and professor of chemical engineering and materials science and biomedical engineering, develops tools, technologies and methods to empower immuno-engineering research and create transformative cancer therapies.
- Keyue Shen, associate professor of biomedical engineering, focuses on cancer cell behavior and metastasis. He recently received a $2 million grant from the National Institutes of Health to understand the spread of cancer leading to secondary growth. The aim: to develop therapies that suppress a cell’s transition from dormant to malignant.
- Eun Ji Chung, the Dr. Karl Jacob Jr. and Karl Jacob III Early-Career Chair, is an emerging leader in nanomedicine. Her lab creates engineered nanoparticles that can target specific areas of the body to treat diseases including cancer, atherosclerosis and kidney disease.
Building Even Better Cancer Treatments with the Help of “Natural Killers”
The next generation of cell-based cancer therapies will need to be even more powerful. For Stacey Finley, math is the master key that will unlock them.
“We build mathematical models, and we’re interested in studying cells using math to make predictions about how the cells will behave,” said Finley, the Nichole A. and Thuan Q. Pham Professor in the Mann Department of Biomedical Engineering.
In the immunotherapy space, Finley creates computer-simulated experiments predicting how cells will respond to treatments. She is interested in signaling pathways — how cells communicate with each other using proteins that latch onto a receptor on the surface of another cell.
Finley is working closely with Nick Graham, an associate professor in the Mork Family Department of Chemical Engineering and Materials Science, on a new project harnessing one of our most formidable immune soldiers: the natural killer cell.
These white blood cells are among the first line of defense during infection and disease. They are smart enough to differentiate between healthy and diseased cells, targeting the harmful ones and secreting a substance — cytokine — to kill them. They also communicate with other immune cells to attack the invader.
“We’re trying to understand the signaling pathways that activate inside natural killer cells. We’re trying to see how the receptors that natural killer cells naturally express work to activate the cells,” Finley said.
By using mathematical modeling and measuring proteins in the signaling pathways of the cells, Finley and Graham hope to engineer powerful new CARs tailored for use in natural killer cells.
Current FDA trials have seen success with lymphoma and leukemia using CAR T-cells derived from naturally occurring T-cell receptors. CAR T-cell treatments are developed from T-cells taken from each patient, an expensive and labor-intensive process. Finley and Graham predict that using natural killer cells as the vehicle instead could provide significant advantages, such as cheap, accessible, off-the-shelf therapies.
“With natural killer cells, there’s the potential that one pool of cells could be given to many different patients because people have a greater tolerance for them, and there is less potential for immune rejection,” Graham explained.
The team’s project focuses on applications for multiple myeloma, which has seen some limited successes in patients with CAR T-cell treatments, but where many approved immunotherapies have not worked well.
“A lot of those successes have been built on a trial-and-error approach, so we’re trying to bring a systematic, data-driven engineering perspective to how to design these,” Graham said.
New Research Alliances to Destroy Silos and Defeat Disease
For game-changing treatments to make it from lab to patient, collaboration is key. Wang is passionate about strengthening research partnerships between USC Viterbi, the Keck School of Medicine and Los Angeles hospitals — building a direct pipeline from the Mann Department’s cell-based engineering research.
Caryn Lerman, director of USC Norris and associate dean for cancer programs in the Keck School of Medicine, shares Wang’s commitment to building a multidisciplinary network of researchers and clinicians making game-changing cancer treatments a reality.
“We are a cross-university cancer center based in the Keck School of Medicine. Our members cross six different schools, including many from Viterbi. We incentivize team science through cross-cutting initiatives, including the development of novel cellular therapies for cancer in collaboration with our colleagues at Children’s Hospital of Los Angeles,” Lerman said.
Keck Medicine of USC and CHLA recently launched the USC-CHLA cGMP Laboratory facility — a cutting-edge manufacturing space for cell and gene therapies. Lerman said it was one example of the progress USC is making in the cancer immunotherapy field.
“We could lead in basic science and engineering in cancer cell therapy, but unless we can translate the research into clinical trials of novel therapies, we will not impact our patients,” Lerman said.
Lenz added that USC is well positioned to play a major role in the development of immune therapies using cell-based or CAR T-based treatments. He said the new cross-disciplinary partnerships harnessing biomedical engineering and artificial intelligence offered a promising future for immunotherapy research and clinical applications at USC.
“We are very excited to have all these options available within our own cancer center,” Lenz said. “We are particularly excited to finally work with Viterbi, and with Peter Wang in this position I think the opportunities are endless. It’s just the beginning of an incredible outlook for the years to come.”
A New Hope for Patients
As USC’s interdisciplinary research breaks new ground in cell-based immunotherapy, cancer patients like Clauer will soon have even more options to help their immune systems fight back.
And Clauer is excited for the future. She is a fierce cheerleader for the medicine that has retrained her body’s immune cells into a cancer-fighting army.
As a patient advocate through the nonprofit Colontown, Clauer offers colorectal cancer patients support, advice and access to evidence-based research. She runs workshops to help them navigate the latest medical trials that may offer them the same hope she has found.
“I’m so grateful to my body. But obviously I’m grateful for the science and engineering and everything that happened to create these treatments,” Clauer said. “What they’re doing is basically redirecting your body to fight the disease. You have a body that somewhat failed you by getting cancer in the first place, but now these drugs can use your own body to heal you. That is amazing to me.”